
Kawasaki disease and Covid-19 - Update January 2022
Authors: Dr Laurent Fermont
(Shaare Zedek Medical Center–Jerusalem–Israel)
Published date: 27 January 2022
Ref: 0727
The SARS-Cov-2 (Covid-19) virus officially appeared in China in December 2019. Although a member of the known family of coronaviruses, it is a newcomer whose virological, epidemiological, clinical and prognostic characteristics are gradually apprehended. At each stage, we have witnessed a succession of news published too quickly by the news media, discussed without filter by doctors not always competent in this specific field, relayed by social networks, often invalidated after a few weeks, and then sources of disturbing rumours.
During the month of April 2020, pediatric services in Lombardy (1), the epicenter of the Covid-19 pandemic in Europe, published alerts about children who allegedly developed “Kawasaki disease” concomitantly with a Covid-19 infection. These reports were quickly confirmed in Paris, including in very young infants <3 months (2.3), London (3) and Washington (5).
It is therefore necessary to focus on the facts and answer legitimate questions:
-
How to define Kawasaki disease? Is this disease serious?
-
Is there a relationship between Kawasaki disease and the Covid-19 pandemic?
-
What advice can you give to obviously worried parents and those around them?
A) Kawasaki disease (6)
It is an acute multisystemic vasculitis that can affect all small and medium-sized arteries, but above all the coronary arteries. It can be diagnosed at any age of childhood and adolescence, mainly infants and young children, mostly boys, aged under 5 years (80% of cases), rarely before 3 months, which leads to assume the existence of maternal immunological protection.
It has become the first cause of heart disease acquired in childhood in developed countries, and the second vasculitis after rheumatoid purpura.
The diagnosis is considered from clinical signs that appear suddenly in an inflammatory atmosphere, in children most often without comorbidity, but comorbidity (any heart, respiratory or kidney disease, any chronic disease considered serious such as diabetes or arterial hypertension, any immune deficiency, any morbid condition such as diabetes) obviously worsens the prognosis.
We still do not know the cause: probably infectious, although to date no agent has been specifically identified. This hypothesis can be retained above all because of its seasonality (late winter and spring), its epidemiological characteristics, lympho-cutaneous-mucous signs suggestive of infectious diseases.
The importance of the biological signs of inflammation points towards an over-activation of the immune system, including the description of true "cytokine storms" induced by an infection (as has been described in the case of infections by respiratory viruses or enteroviruses) and conferring a logic that has led to the prescription of anti-inflammatory, immunological and sometimes anticoagulant treatments that have proven their effectiveness.
Although described in 1967 in Japan (with a first case in France published by G.Brévière in 1979) (7), this disease remains mysterious in many respects.
Rare in Europe and the United States (10 to 20/100,000 depending on the country), it is fifteen to twenty times more frequent in Japan and in other countries of the Far East, which has led to assume that it is influenced by environmental, geographical (8) but also genetic factors. Several genes involved in the immune response of Japanese and Western populations have been identified, including two main genes allowing to explain the mechanism of action of immunoglobulins, still partially understood, and the involvement of innate immunity: these are FCGR2A encoding the receptor II region of the FC fraction of gammaglobulin (9), and ITPKC encoding the regulation of T cell activation (10).
Clinical criteria lead to the evocation of the diagnosis (11, 12) in the absence of a pathognomonic test.
A fever with photophobia, appearing suddenly, rebel to the usual treatments, and it is agreed to think of Kawasaki disease in front of a child whom fever persists for more than four days (Day 1: onset of fever).
Non-purulent and antibiotic-resistant cervical lymphadenopathy.
Cutaneous signs: characteristic morbilliform or scarlet fever-like exanthema affecting the trunk, limbs, face and perineal regions, palms of the hands and soles of the feet with, especially, edema of the backs of the hands and feet. A palmar, plantar and peri-ungual desquamation is observed during the evolution.
Mucosal signs: bilateral conjunctivitis, cheilitis with dry cracked lips, oral enanthema and pharyngitis,
Non-specific signs: digestive signs (pain, diarrhoea, vomiting), arthralgia, neurological and meningeal signs, hepatic insufficiency and cytolysis, pneumopathy and breathing difficulties, collapse. These signs, even dissociated but in a prolonged febrile atmosphere and without a surgical context, are evocative. We conceive the difficulty of the diagnosis especially if they are degraded or isolated, making then speak of “incomplete form of Kawasaki disease”.
The diagnosis of complete form of Kawasaki disease should therefore be considered in the event of an intractable febrile state after four days of treatment, if at least four of these signs are observed.
Laboratory tests confirm the inflammatory nature of the disease. With the usual signs (CRP>30mg/L, SR>40mm in the first hour), hyperleukocytosis with a special mention for thrombocytosis, particular by the importance of its level often >800,000/mm3 so frequent after the first week.
Since 2004, partial, so-called “incomplete” forms have been described (10). The children are a little older (6-8 years old). We should certainly not hesitate to consider an incomplete form as soon as three or even only two of the clinical and inflammation signs mentioned above are present in a child who has been febrile for five days (or even four!) despite all the treatments implemented. The diagnosis of these degraded and incomplete forms is often difficult (12), which explains the possibility of diagnostic delays.
However, the hypothesis of a diagnosis of Kawasaki disease directly leads to fear of cardiac involvement, both a sign and a complication of this disease, even in clinically degraded forms. Prescribing the recommended treatments as early as possible has the advantage of preventing cardiac damage before it occurs, or of treating it under better conditions if the child suffers from it at the time of diagnosis.
The electrocardiogram can show diffuse non-specific repolarization disorders but also, in 10% of cases, atrioventricular conduction disorders, generally 1st degree.
Doppler echocardiography is, as everyone knows, a non-invasive examination particularly suitable for children, and it is available everywhere. At the slightest doubt of Kawasaki disease, whether the clinical form is complete or incomplete, ultrasound examinations which will support the diagnosis must be requested urgently (10,11).
The coronary arteries must be checked, since they can be affected within three weeks of the onset of the disease (Figure 1). The data will be interpreted according to the reference curves available (10).
These arteries can be dilated with an often hyperechoic and thickened wall, and sometimes the presence of aneurysms (25% of untreated forms).
These aneurysms can be single or multiple, and involve one or both coronary arteries. Variable in size,< 1-2mm to > 8mm (we then speak of a giant aneurysm), they can be single or multiple, sometimes in a string (12, 13).
Left ventricular dysfunction may be secondary to coronary thrombosis and ischemia, but in the acute phase it is mostly myocarditis, which is not surprising in this inflammatory and probably infectious disease.
Echocardiography can also reveal valvular and pericardial involvement. It makes it possible to follow the evolution of the cardiac function and the pulmonary pressures in the event of pneumopathy and respiratory insufficiency.
The coronary scanner analyzes myocardial damage and visualizes the entire coronary and aortic network. All the middle arteries can be affected and the scanner can usefully complement the echocardiography to assess the disease, even if the prognosis really depends on the coronary state.
Treatment (11,12)
Limitation and regression of coronary anomalies are possible. This is especially true if the treatment takes place within the first 10 days of the illness (Day 1 of the fever). The precocity of the diagnosis, and of the implementation of the treatment, is thus the key to its effectiveness and to the prevention of coronary damage, and possible cardiological complications in the long term.
It is therefore an imperative, relating Kawasaki disease to a medical emergency.
There are indeed effective treatments to combat inflammation, but also to prevent the occurrence of coronary signs (<5% of cases treated in time vs 25%).
As soon as possible - in the first week following the onset of the disease (Day 1 of the fever) - the child must have an intravenous administration of immunoglobulins (IgG) (2g/kg). Resistance may lead to an indication of second administration. Acetylsalicylic acid (80-100mg/kg) is added, remembering that ibuprofen should be avoided.
In 85% of cases, early treatment will result in a rapid reduction in fever and inflammatory signs.
In case of inefficiency, hemolytic anemia can occur (15%), we will then turn to other routes. These are corticosteroids (3mg/kg/24h) for three days, which originally seemed "counter-intuitive", but whose logic has appeared since the description of the "cytokine release syndrome", as well as TNF alpha inhibitors or monoclonal antibodies (infliximab).
In case of early coronary involvement, the child will have every chance of recovering a normal coronary network if treatment is started within the first seven days. These chances will be all the greater for simple dilatations of the arteries or small aneurysms (<2 mm).
The observation of a normal coronary network will authorize the discontinuation of acetylsalicylic acid after six weeks. Several years of obligation to prolonged treatments, sports limitations, cardiological prognostic uncertainties, will thus be avoided, and will protect these children against complications related to thrombosis and remodeling of the arteries.
If the treatment was started beyond the tenth day, the coronary risk is increased and the chance of obtaining a regression of the “medium” or “giant” aneurysms (>8mm) is more random and more delayed.
If the regression is clear but incomplete, the heparin anticoagulants of the acute phase will be replaced by an “acetylsalicylic acid–clopidrogel” combination. This is obviously positive when we know the difficulties of handling prolonged prescriptions of anticoagulants and vitamin K antagonists in young children.
If large (>4mm) or giant (>8mm) coronary aneurysms persist, anticoagulants should be maintained. They will eventually be associated with preventive treatments with beta-blockers or ACE inhibitors. Indications for surgical revascularization in young adults will sometimes also be essential.
B) Kawasaki disease and Covid-19
It is apparent from the above that Kawasaki disease is a serious disease. It is urgent to think about it, especially in times of epidemic or infectious endemic, as has been the case since 2019 and the appearance and generalization of Covid-19.
It is understandable that the news of an increase in cases in geographical areas hit by the ongoing pandemic has raised concerns in pediatric circles.
A direct link does indeed seem to exist between Kawasaki disease and Covid-19:
-
A link between Kawasaki disease and a coronavirus epidemic has already been considered as early
as 2005 (15). -
In times of a virulent pandemic, it is extremely worrying to find a number of children suffering from "Kawasaki-type" illness that is significantly higher than the expected number. Our Italian colleagues estimate that the frequency of Kawasaki disease was 30 times higher than the expected frequency.
This is also what was observed in Paris since Pr. Damien Bonnet (Necker) reported many cases over a period of less than a month whereas, in a usual situation, the frequency of Kawasaki disease diagnoses n not exceed one case per month. -
In addition, as in Kawasaki disease, an ethnic African and West Indian predisposition is observed in France, and in the United States, Hispanic and Afro-American.
-
A French and Swiss collaborative study has been published under the aegis of Pr. Damien Bonnet (Necker-Paris) (3). It concerns 35 children infected with Covid-19 (bacteriological positivity in 88%), who developed cardiac involvement with myocarditis and significant left ventricular dysfunction.
All of the children in this group, older (7 years) than in the usual Kawasaki disease setting, survived, including those who showed signs of high severity and had to be treated with extremely heavy resuscitation measures, since oxygenation by extracorporeal membrane (ECMO) was necessary in 28% of them. In addition, left ventricular function remained impaired at discharge from the intensive care unit in 10/35 children. This direct relationship has also been confirmed in Italy, the epicenter of the pandemic in Europe. -
There is a clear epidemiological notion of infectious disease, since 70% of the children in question had contact with people around them diagnosed as positive by PCR.
However, notable differences led to the individualization of a particular entity (17) comprising an average age of Covid patients of 7 years, therefore higher than classic Kawasaki patients, different biological profiles, uncertainties on the risks of prolonged deficiency, in particular pulmonary or immunological. A big difference is the notion of a clearly identified infectious etiology of MISC, with its corollary of the possibility of vaccination, which has the enormous advantage of protecting patients from serious forms. Widely approved and favored in case of comorbidities, widely accepted in young people over 12 years old, it remains discussed to this day in children aged 6 to 11 years without comorbidities. Promoted in the United States, including for this last category due to the high mortality (more than 1,000 deaths in December 2021), accepted in Israel, there is a reluctance in France in the absence of risk factors, and where the pediatric care conditions are very different.
Conclusion
Despite diagnostic criteria, risks and common practices, two entities are currently described, namely traditional Kawasaki disease, and Multisystem Inflammatory Syndrome in Children (known as "MIS-C“) via Covid-19 infection. From 2 March 2020 to 30 December 2021, Santé Publique France reported 826 cases of MIS-C, 80% directly related to Covid 19 infection (18).
It is absolutely necessary to be informed of this association in order to be able to prescribe the recommended treatments quickly, without loss of time and opportunity. This is all the more true as the profile of a second wave could differ due to a modification of the virus, an association of several infectious agents (16), or a modification of the clinical profile of the disease, as was the case during the Hong Kong (H3N2) flu pandemic of 1968-1970, where younger patients were more severely affected in the 'second wave'.
Consequently, a principle should be remembered by all caregivers caring for children, especially during the SARS-Cov-2 pandemic period:
-
Kawasaki disease should be considered a medical emergency. This is also the case for MISC/PIMS.
-
A stubborn fever of more than four days accompanied by any sign should suggest this diagnosis.
-
This must direct the patient, urgently, to a specialized pediatric consultation, a cardiological consultation with echocardiography-doppler, before a multidisciplinary discussion can validate the diagnosis of Kawasaki disease or MISC-C /PIMS, and initiate the processing.
_______________________________________
Bibliography
-
L. Verdoni et Coll. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic:an observational cohort study. The Lancet 2020 (May 13):396
-
N.Nathan et Coll. Atypical presentation of COVID-19 in young infants. The Lancet 2020;395:1481
-
Z.Belhadjer et Coll. Acute heart failure in multisystem inflammatory syndrome in children (MIS-C) in the context of global SARS-CoV-2 pandemic. Circulation, 2020 (May 19);141
-
S. Rhippagen et Coll. Hyperinflammatory schock in children suffering from Covid-19. The Lancet;395:1607
-
RL. DeBiasi. Severe COVID-19 in Children and Young Adults in the Washington, DC Metropolitan Region. J.Pediatr. 2020 (May 13);220
-
R. Cimaz et Coll. La maladie de Kawasaki. Rev Prat et Orphanet 2007;57:1985-1988
-
GM Bréviere. Le syndrome adeno-cutanéo-muqueux avec atteinte pulmonaire. Archives françaises de Pédiatrie, 1979;36:182-187
-
JC Burns et Coll. Seasonality and Temporal Clustering of Kawasaki Syndrome. Epidemiology 2005;16:220-225
-
Khor C et Coll. Genome-wide association study identifies FCGR2A as a susceptibility locus for Kawasaki disease. Nat Genet 2011;43:1241-1246
-
Onouchi Y et Coll. ITPKC functional polymorphism associated with Kawasaki disease susceptibility and formation of coronary artery aneurysms. Nat Genet 2008;40:35-42
-
Newburger et Coll. Diagnosis, treatment, and long-term management of Kawasaki disease:a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease, Council on Cardiovascular Disease in the Young. Circulation 2004;110:2747-71.
-
McCrindle et Coll. Diagnosis treatment and long-term management of Kawasaki disease. Circulation 2017;135:927-99
-
A. Harahsheh. Missed or delayed diagnosis of Kawasaki disease during the 2019 coronarovirus disease (Covid-19) pandemic. J.Pediatr. 2020 (April 23th)
-
K.Friedman et Coll. Coronary Artery Aneurysms in Kawasaki Disease: Risk Factors for Progressive Disease and Adverse Cardiac Events in the US Population. JAHA Sept 2016 Vol5-Nb.
-
F.Esper et Coll. Association between a Novel Human Coronavirus and Kawasaki Disease. J. of Infectious Diseases 2005;191:499-502
-
E.Payan et Coll. SARS-Cov-2 and influenza virus coinfection. The Lancet 2020 (May 05):395:1587
-
MK Siebach et Coll. Covid 19 in Childhood:T ransmission, clinical presentation, complications and risk factors. Pediatric Pulmonology 2021;56:1342-1346
-
Surveillance des cas de syndrome inflammatoire multisystémique pédiatrique. Santé Publique France, Bilan au 30 décembre 2021
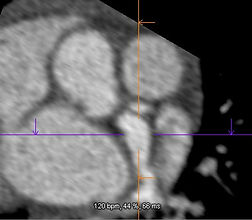
FIGURES: Coronary damage
Figures 1 a and b. Echocardiography
-
a-Echocardiography: dilation of the left coronary common trunk
-
b-Echocardiography: proximal right and left coronary aneurysms
Figure 2: Scanner
Coronary scanner - Aneurysms
Dr Max Godfrey; Shaare Zedek Medical Center Jerusalem-Israel
![l_maladie_kawasaki[1].jpg](https://static.wixstatic.com/media/c2ab67_d5ceaa02032743d2adc13f3cb1377323~mv2.jpg/v1/fill/w_452,h_153,al_c,lg_1,q_80,enc_avif,quality_auto/l_maladie_kawasaki%5B1%5D.jpg)



_edited_edit.jpg)


